Critical Care
The Southwest Journal of Pulmonary and Critical Care publishes articles directed to those who treat patients in the ICU, CCU and SICU including chest physicians, surgeons, pediatricians, pharmacists/pharmacologists, anesthesiologists, critical care nurses, and other healthcare professionals. Manuscripts may be either basic or clinical original investigations or review articles. Potential authors of review articles are encouraged to contact the editors before submission, however, unsolicited review articles will be considered.
Ultrasound for Critical Care Physicians: Unchain My Heart
William Mansfield, MD
Michel Boivin, MD
Division of Pulmonary, Critical Care and Sleep Medicine
Department of Medicine,
University of New Mexico School of Medicine
Albuquerque, NM USA
A 46-year-old man presented after a motor vehicle collision. He suffered abdominal injuries (liver laceration, avulsed gall bladder) which were successfully managed non-operatively. The patient remained intubated on mechanical ventilation and remained hypotensive after the injuries resolved. The patient required norepinephrine at low doses to maintain a normal blood pressure. It was noted the patient had a history of remote tricuspid valve replacement. A bedside echocardiogram was then performed to determine the etiology of the patient’s persistent hypotension after hypovolemia had been excluded.
Video 1. Apical four chamber view centered on the right heart.
Video 2. Apical four chamber view centered on the right heart, with color Doppler over the right atrium and ventricle.
Video 3. Right ventricular inflow view.
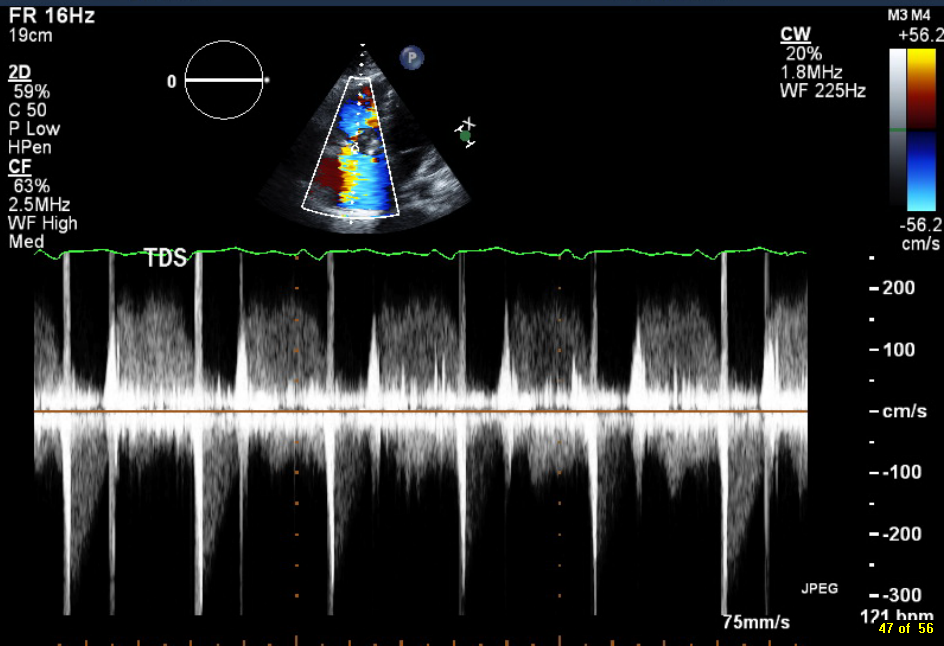
Figure 1. Continuous-wave Doppler tracing through the tricuspid valve.
What tricuspid pathology do the following videos and images demonstrate? (Click on the correct answer to proceed an explanation and discussion)
Cite as: Mansfield W, Boivin M. Ultrasound for critical care physicians: unchain my heart. Southwest J Pulm Crit Care. 2017;14(2):60-4. doi: http://doi.org/10.13175/swjpcc013-17 PDF
Ultrasound for Critical Care Physicians: Hungry Heart
A 31-year-old incarcerated man with a past medical history of intravenous drug use and hepatitis C, presented with a one week history of dry, non-productive cough, orthopnea and exertional dyspnea. He denied current intravenous drug use, and endorsed that the last time he used was before he was incarcerated over 3 years ago, his last tattoo was in prison, 6 months prior. He was found to have an oxygen saturation of 77% on room air, fever of 40º C, heart rate of 114 bpm, and blood pressure of 80/50 mmHg. The patient had a leukocytosis of 14 x109/L, and a chest x-ray demonstrating patchy airspace disease. Blood cultures were sent and he was treated with antibiotics and vasopressors for septic shock. The patient was intubated for acute hypoxemic respiratory failure secondary to multifocal pneumonia. A bedside transthoracic echocardiogram was performed.

Figure 1. Apical four chamber view echocardiogram with color Doppler over the mitral valve.

Figure 2. Right Ventricular (RV) inflow view echocardiogram from same patient What is the likely diagnosis supported by the echocardiogram? (Click on the correct answer for an explanation)
Cite as: Villalobos N, Stoltze K, Azeem M. Ultrasound for critical care physicians: hungry heart. Southwest J Pulm Crit Care. 2016;12(1):24-7. doi: http://dx.doi.org/10.13175/swjpcc007-16 PDF

